Summary
- There are two ways to approach HIPAA compliant medical forms, one is, forms like patient intake forms and consent forms that must follow HIPAA guidelines, and second, forms that are mandatory to maintaining HIPAA compliance within an organization like authorization forms, and business associate agreements (BAAs).
- Both are mandatory for healthcare providers, health plans, clearinghouses, business associates, medical labs, and pharmacies to protect sensitive patient data and avoid hefty penalties.
- Transitioning to online HIPAA compliant forms helps streamline processes, ensures proper documentation, facilitates compliance, and enables secure sharing of protected health information (PHI).
In 2022, the healthcare industry bore witness to 344 instances of data breaches, exposing the vulnerability of patient information. Among these breaches, a devastating cyber attack in the health insurance sector compromised a staggering 78.8 million private records.
Beyond financial implications, such breaches put patient health at risk and critical medical data becomes inaccessible when needed. HIPAA was established in the US in 1996 to help navigate through such threats, safeguarding patient medical information and enforcing the ramifications of non-compliance.
In today’s digital era, processes such as data collection, payments, and storage have completely transitioned to online platforms, and healthcare is no exception. With healthcare organizations opting for digital forms to collect patient information, collect payments and store patient information, the need for HIPAA-compliant forms cannot be overstated. These forms serve as vital guardians of patient privacy and healthcare integrity.
If you are a professional working in the medical or healthcare industry in the US, looking to understand HIPAA compliant forms for your organization, this blog is your ultimate guide.
Let’s start with the basics, What is HIPAA, what are HIPAA compliant forms, and what are its components. We’ll then dive into the various types of HIPAA forms, types of companies that need to comply with HIPAA, companies that don’t need to do so, and consequences on non-compliance.
Read on to know everything you need to know about HIPAA-Compliance forms.
What is HIPAA and Why Does it Matter?
Health Insurance Portability and Accountability Act, or HIPAA, of 1996 is a legislation that outlines security and data privacy provisions for keeping medical information safe and secure.
It imposes a mandate on the establishment of national standards on organizations to safeguard patient health information from being used or disclosed without the knowledge or consent of patients.
HIPAA compliance means the compliance of an organization with a set of security regulations established by the Health and Human Services (HHS) department of the US.
But why is HIPAA important?
The set of rules created by HSS in HIPAA include robust technical, administrative, and physical security measures to effectively protect patient information and their medical records. These rules have to be followed by healthcare businesses that digitally or electronically transmit sensitive data.
What exactly are HIPAA Compliant Forms?
So, there are two key perspectives to HIPAA-compliant forms.
- First, any digital form used to collect patient information at a healthcare or medical organization must adhere strictly to the guidelines outlined in HIPAA regulations. For example, medical history questionnaires, consent forms for treatment, and patient intake forms. All such types of digital forms must comply with HIPAA regulations to protect patient privacy and data security.
- And second, there are forms that are mandatory for maintaining HIPAA compliance within an organization. For example, privacy notices, HIPAA authorization forms, and business associate agreements (BAAs). These forms are critical for making sure that the organization meets its legal obligations and protects patient information effectively.
Let’s start with –
A. Forms for Collecting Patient Information (That Have To Strictly Adhere to HIPAA Guidelines)
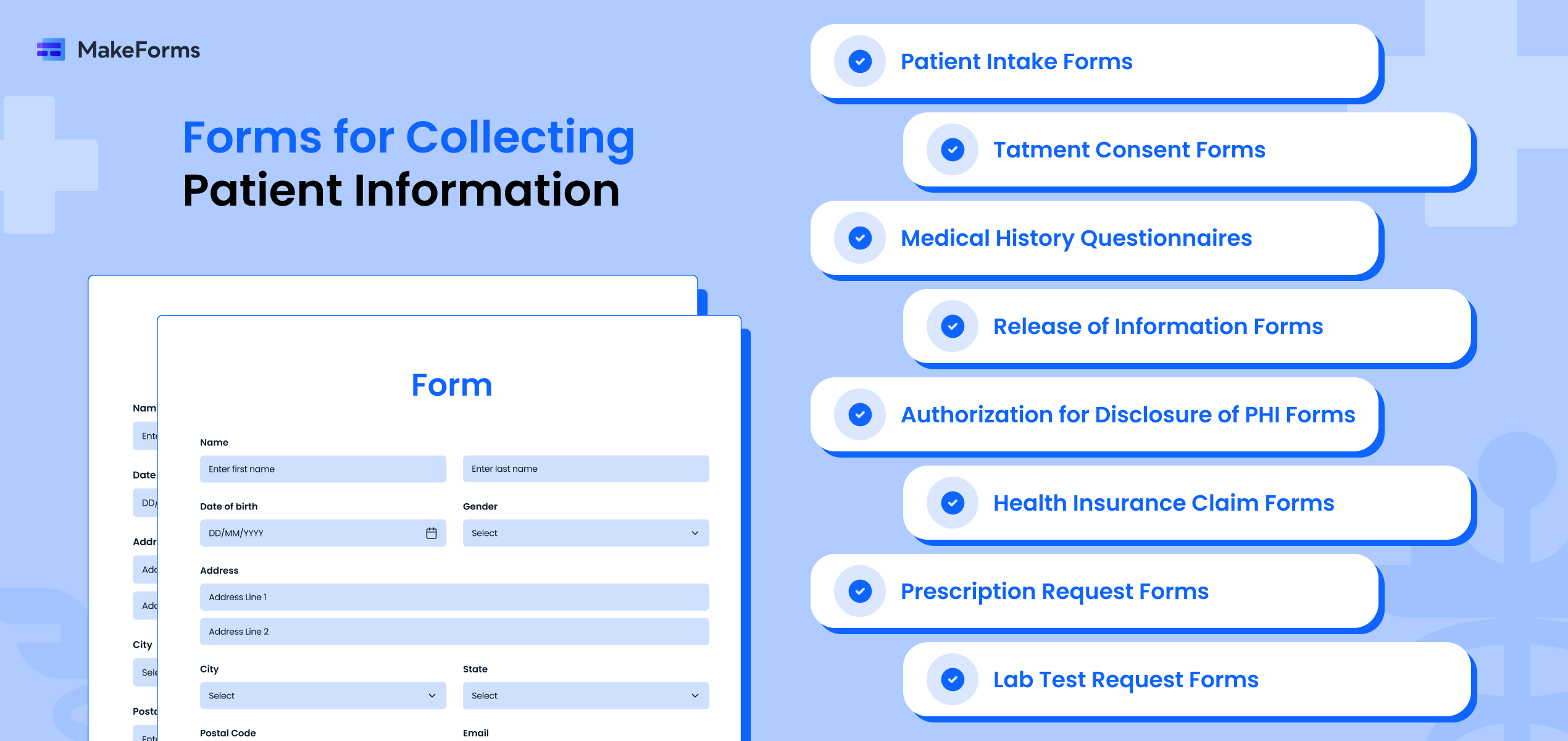
Patient Intake Forms
Electronic patient forms collect basic information needed about new patients. These forms streamline the intake process and enhance the patient experience. The forms also help understand the purpose of a patient’s visit, assess appointment length, and verify their insurance.
Treatment Consent Forms
Consent forms are essential for obtaining a patient’s permission before administering any medical procedure, treatment, or surgery. This form outlines the benefits, risks, and alternatives of the proposed treatment. It ensures that patients are informed and can make decisions about their healthcare based on the same.
Medical History Questionnaires
Medical history questionnaires delve deeper into a patient’s health background. It covers the patient’s any past illnesses, current symptoms, lifestyle (e.g., alcohol or smoking consumption), surgeries, and family medical history. They help understand a patient’s overall health status and potential risk factors.
Release of Information Forms
These forms authorize the release of a patient’s medical information to specified individuals or entities, like legal representatives, insurance companies, or other healthcare providers. Patients must provide consent for their protected health information (PHI) to be shared.
Authorization for Disclosure of PHI Forms
Just like release of medical information forms, authorization forms specifically grant permission for the disclosure of PHI for purposes not covered by treatment, payment, or healthcare operations. This includes the sharing PHI for marketing, research, or other non-standard uses.
Health Insurance Claim Forms (For example: CMS-1500)
These forms are used to submit claims for the seamless reimbursement from health insurance companies for medical services provided to patients. Health insurance claim forms include details such as patient demographics, diagnosis codes, dates of service, procedure codes, and provider information.
Prescription Request Forms
These forms are used by patients to request prescription medications from their healthcare providers. They typically include the patient’s information, the medication name, dosage instructions, refill requests, or any special precautions/instructions.
Lab Test Request Forms
Lab test request forms are used to get specific laboratory tests or diagnostic procedures for patients. These forms must specify the type of test, patient information, reason for the test, and any additional instructions for sample collection or preparation.
Referral Forms
When a healthcare provider refers a patient to another healthcare facility or specialist for further evaluation, treatment, or services, referral forms are used. These forms generally include details about the patient information, referring provider, the reason for referral, and any pertinent medical history.
In order for the above forms to be compliant with HIPAA, there are certain guidelines that need to be followed. Let us now look at those critical guidelines.
Guidelines That Must Follow to be HIPAA Compliant Medical Forms
The medical forms discussed above need to adhere to multiple key aspects of compliance to ensure the complete protection and security of patients’ sensitive health information.
Here are the crucial types of compliance requirements that these forms must meet under HIPAA:
- Privacy and Security: Forms that are used for collecting, transmitting, or storing ePHI must implement appropriate safeguards. These include access controls, encryption, audit trails, and secure storage to safeguard data against unauthorized access, breaches, and cyber threats.
- Patient Authorization: Some forms, like Authorization for Disclosure of PHI or Release of Information, must comply with HIPAA’s requirements for patient authorization. This includes obtaining patient consent before disclosing PHI to third parties. They also need to clearly specify the purpose and scope of the disclosure.
- Minimum Necessary Standard: HIPAA’s Minimum Necessary Rule requires covered entities to limit the use, disclosure, and request of PHI to the minimum necessary to accomplish the intended purpose.
- Business Associate Agreements: If forms involve any business associates or third-party entities that manage PHI on behalf of a covered entity, HIPAA-compliant forms must include provisions for BAAs. These agreements lays out the responsibilities of the business associates in securing PHI and complying with HIPAA regulations.
- Documentation and Recordkeeping: HIPAA mandates covered entities to maintain documentation that demonstrates compliance with the Privacy, Security, and Breach Notification Rules. This includes maintaining records of patient authorizations, risk assessments, security measures implemented, training records, policies and procedures, and incident response plans related to PHI.
B. Forms mandatory for maintaining HIPAA compliance within an organization
Now that we have covered medical forms that must adhere to HIPAA rules and what those guidelines are, we move onto forms and other regulations that are mandatory for maintaining HIPAA compliance within an organization.
1. HIPAA Authorization Forms:
HIPAA authorization forms are used to share patient health data with external parties for multiple purposes. There are several types of authorization forms used by medical organizations, and all these forms must comply with the all HIPAA regulations:
I. New Patient Authorization Form
This is generally a standard intake form for collecting basic information about the patient.
It includes:
- Basic patient demographics
- Their insurance details
- And communication preferences
Medical organizations leverage this form to verify and get details of the patient’s insurance coverage.
II. Medical Release Form
Medical release forms help in maintaining patient health confidentiality. This authorization form needs to be filled before sharing medical information of patients with anyone other than the patient itself, health insurance companies, pharmacies, or their legal representative. Medical release forms are a mandate in the following scenarios:
- when sharing PHI with universities for research/educational purposes
- when disclosing psychotherapy notes
- when the physician leaves the organization but continues to treat the patient
- when highlighting patient recovery stories for marketing
III. Authorization for Use/Disclosure of PHI for Marketing
This form is required under HIPAA if a covered entity wants to use or disclose a patient’s protected health information for marketing purposes, like newsletters, promotional materials about new services, or communications about purchase or use of products/services.
This form needs to specify exactly what PHI will be used for marketing, for e.g.:
- Name
- Contact information
- Diagnosis
- And how it will be used in marketing communications
Marketing Authorization form requires specific elements like a description of the intended marketing and an expiration date.
The authorization must clearly define if the marketing involves financial remuneration to the covered entity from a third party. The form should also include statements about the patient’s rights, for e.g. patients’ right to revoke this authorization at any time.
IV. Research Authorization Form
Researchers need to obtain signed authorization from patients to access, disclose, or use PHI for research purposes. This form describes the specific research study/protocol and how the patient’s PHI will be used and disclosed.
It also specifies if PHI contains:
- Identifiable,
- De-identified, or
- Fully anonymized information
The form must outline if PHI will be re-disclosed to other entities fr individuals outside the research and for what purposes.
2. Notice of Privacy Practices (Privacy Notices):
Privacy notices are documents provided to patients that explain their rights regarding their PHI, how their information may be used or disclosed, the healthcare provider’s responsibilities for protecting their privacy, and how patients can exercise their rights under HIPAA. This notice is typically given to patients during their first visit to a healthcare provider.
3. Business Associate Agreements (BAAs):
This is an agreement between you and an entity or individual that is outside your institution or practice. For example, any cloud service that receives, transmits, stores, or processes PHI would have to sign a HIPAA-compliant business associate agreement with you or your organization. Specifically, if you were to use an online form software or EHR (electronic health record) software these parties would be required to sign a BAA.
A BAA is an acknowledgement of their responsibility to keep protected health information safe. It is also a confirmation that the parties have efficient systems and technology in their organization for the protection of PHI and are HIPAA-compliant.
In the absence of a signed BAA form, covered entities may be held liable for mishandling PHI. They may also face heavy penalties for the same and be asked to take corrective actions for violating HIPAA laws. Hence, this form is a compliance requirement.
4. Security Risk Assessments:
These assessments are evaluations conducted for identifying and mitigating potential risks to the confidentiality, integrity, and availability of Patient Health Information. Security risk assessments help CEs and BAs uncover vulnerabilities in their processes as well as implement proper security measures to protect PHI.
5. Policy and Procedure Manuals:
Policy and procedure manuals outline an organization’s policies, practices, protocols in terms o fHIPAA compliance. It includes policies and procedures on data security, privacy protections, breach response, and employee training. The manual provides guidance to staff members on how to handle PHI safely and in accordance with HIPAA regulations.
6. Incident Response Plans:
Incident response plans are exhaustive strategies developed for addressing and managing data breaches, unauthorized disclosures, and security incidents of PHI. These plans include the steps needed to be taken in case of a breach. For example breach notification procedures, investigation protocols, containment measures, and remediation actions.
7. Data Encryption and Decryption Policies:
Data encryption and decryption policies outline the procedures and standards for securely encrypting sensitive data. It is outlines for PHI both at rest (stored data) and in transit (data being transmitted). These policies make sure that PHI is safeguarded from unauthorized access or interception by encrypting it with the help of strong encryption algorithms.
8. Data Breach Notification Forms:
Data breach notification forms are used for reporting breaches of unsecured PHI to the Department of Health and Human Services (HHS), the affected individuals, and any other entities mentioned in the HIPAA regulations. These forms explain the nature of the breach, the types of PHI involved, mitigation efforts, and steps taken to prevent future breaches.
9. HIPAA Compliance Training Acknowledgment Forms:
These forms are used to affirm that workforce members and/or employees have received training on HIPAA compliance and have acknowledged their complete understanding of HIPAA regulations, security practices, privacy policies, and their responsibilities regarding PHI. Acknowledgment forms helps in demonstrating compliance with HIPAA training requirements.
Types of Organizations Obligated To Use HIPAA Compliant Forms
Contrary to popular belief, HIPAA-compliance is not limited to doctors’ clinics and hospitals. In fact, any organization that collects or deals with PHI has to comply with HIPAA regulations and use only HIPAA compliant forms.
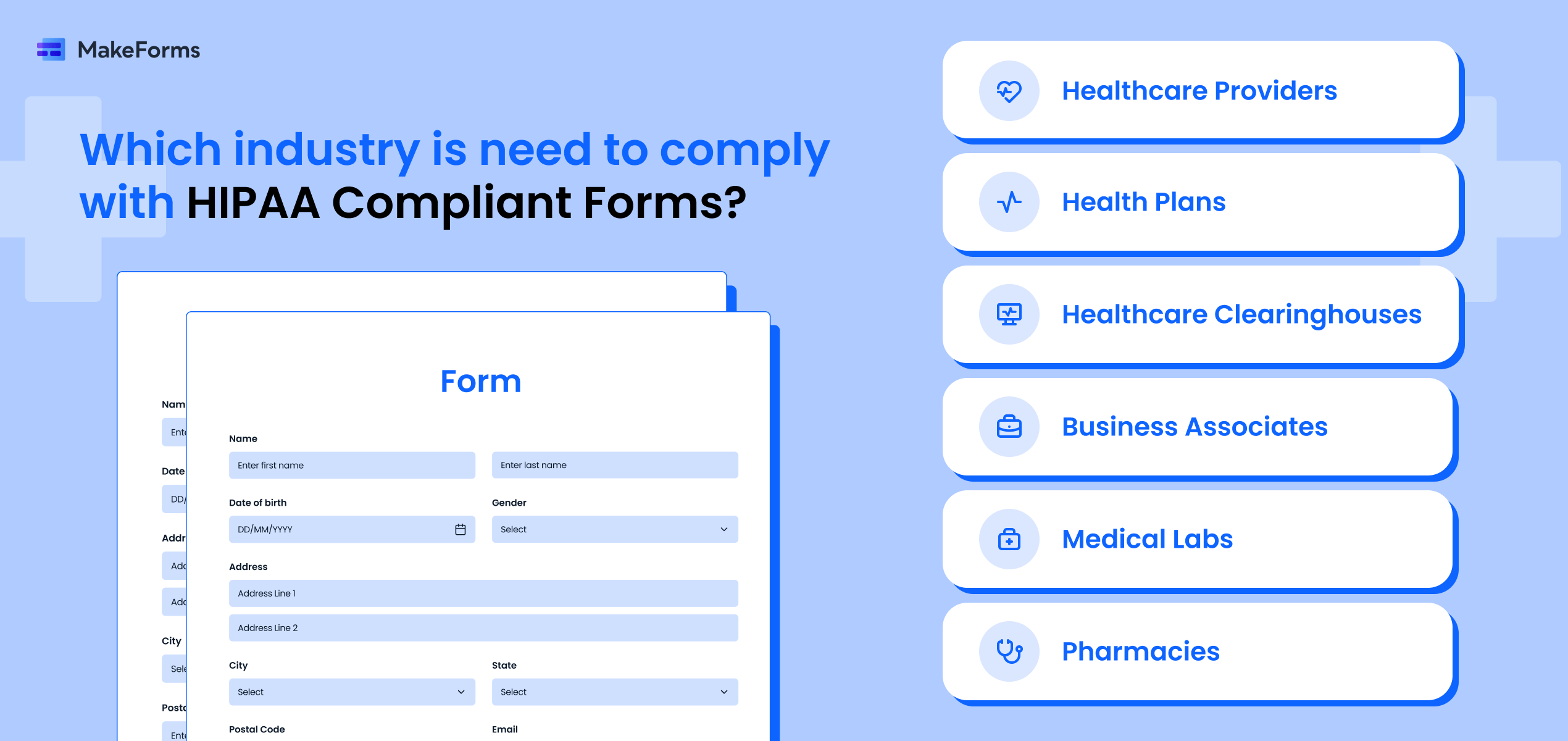
Following are common types of organizations that need to use HIPAA-compliant forms:
- Healthcare Providers: This includes doctors, dentists, nurses, therapists, or any other medical professionals who provide healthcare services.
- Health Plans: Insurance companies, Health Maintenance Organizations, Medicare, and Medicaid. Basically, if they deal with your health insurance, they need to be HIPAA-compliant.
- Healthcare Clearinghouses: Healthcare clearinghouses ensure that data moves securely between patients and healthcare providers. These are the middlemen who process non-standard health information into standard formats.
- Business Associates: Anyone who works with protected health information (PHI) on behalf of a covered entity falls into the category of a Business Associate. This can include IT companies, transcription services, and billing agencies.
- Medical Labs: From blood tests to biopsies, labs handle some of the most personal health data. HIPAA compliance ensures this data collected in medical labs remains confidential and secure.
- Pharmacies: Corner drug stores as well as massive pharmacy chains, all kinds of pharmacies handle sensitive prescription and patient information. This makes HIPAA compliance a must for them.
These are the different types of health institutions that need to be HIPAA-compliant. Using mandatory HIPAA forms is imperative for protecting patient privacy and fulfilling legal obligations.
Neglecting these forms exposes healthcare providers and other covered entities to substantial risks, like very costly penalties. More on the consequences below:
Consequences of Not Having HIPAA-Compliant Forms
Not having or properly using HIPAA compliant forms results in the following serious consequences for healthcare organizations in the United States.
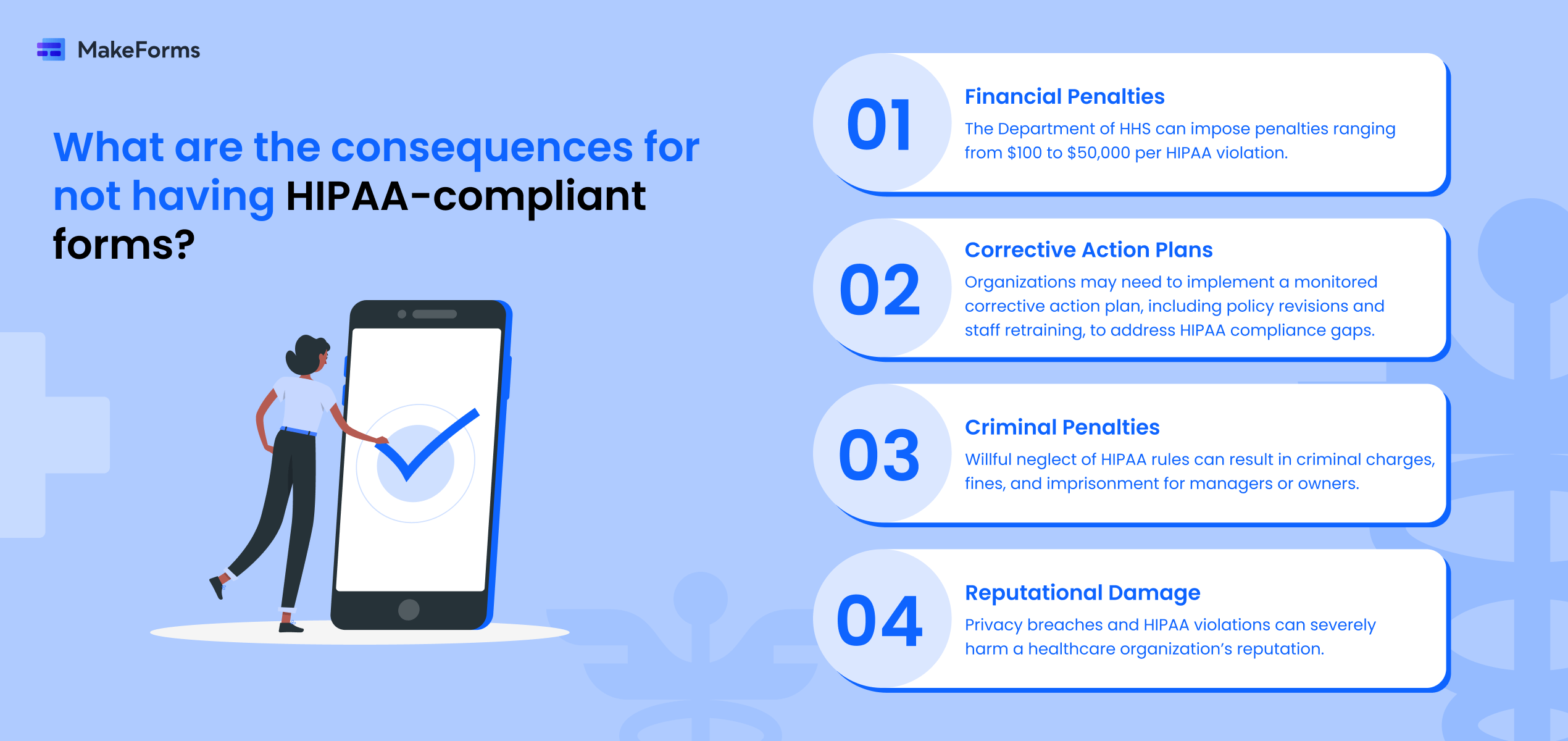
- Financial Penalties: The Department of HHS can impose heavy financial penalties for HIPAA violations that can range from $100 to $50,000 per violation.
- Corrective Action Plans: Organizations may be required to implement a corrective action plan monitored by HHS to address gaps in HIPAA compliance. This could include revising policies, using proper forms, and retraining staff.
- Civil Lawsuits: Patients whose privacy was affected due to lack of compliant forms have the right to file civil lawsuits against the healthcare provider or covered entity seeking compensation.
- Criminal Penalties: If an organization is found willfully neglecting HIPAA rules, its managers or owners could face criminal charges resulting in fines and potential imprisonment.
- Reputational Damage: Privacy breaches and HIPAA violations can severely damage a healthcare organization’s reputation.
You can refer to this website for the latest regulations regarding HIPAA violations.
However, there are certain instances or organizations that don’t require the use of HIPAA-compliant medical forms.
Scenarios Where HIPAA Compliant Forms Aren’t Required
Here are some scenarios or organizations that do not need HIPAA-compliant forms:
- Organizations That Don’t Handle Protected Health Information (PHI): Including Non-medical businesses, schools, and most government agencies that do not deal with PHI.
- Personal Health Records and Fitness Trackers: People’s personal records or fitness data not part of a covered entity’s medical records.
- Employers and Health Plan Records: Employers that sponsor group health plans are not directly subject to HIPAA.
- Law Enforcement and Judicial Proceedings: Agencies or authorities that are acquiring PHI during investigations or legal proceedings.
- Public Health Activities: Public health authorities that collect PHI for specific purposes, like disease prevention.
- Workers’ Compensation Insurers: Entities handling PHI related to workers’ compensation claims.
- De-identified Health Information: Data that has been properly de-identified and cannot be linked to an individual.
Integrating HIPAA Forms into Healthcare Systems in your Medical Organization
Using HIPAA compliant online forms is a no-brainer for eligible organizations; by automating the distribution, collection, and storage of forms, you not only streamline the process but also reduce the chances of human errors creeping in. But seamlessly integrating it into your organization’s healthcare systems is what can make or break the execution.
A few guidelines to follow before switching to online forms are:
- Check for Form Providers that are HIPAA compliant (more on how to check below!)
- Ensure that your existing healthcare systems can smoothly integrate with the chosen form provider.
- Ensure your staff can be trained to use new form systems effectively and securely.
- Conduct regular audits and updates to ensure ongoing compliance with HIPAA regulations.
- Establish clear protocols for data access, sharing, and storage to maintain patient confidentiality.
- Monitor and address any potential security risks or breaches promptly.
Ready to adopt online HIPAA compliant forms for your organization? Amazing! Before you choose a provider, make sure they are HIPAA-compliant, here’s how you can go about it.
How to Check if a Form Provider is HIPAA Compliant
Being certain of your form provider’s HIPAA-compliance is crucial for safeguarding sensitive patient information and avoiding penalties.
Here’s how you can verify their compliance:
- Review their security measures: Scout for encryption protocols for data transmission and storage. Make sure that they employ access controls to limit who gets access to patient data.
- Check for Compliance Certifications: Many reputable form providers will display HIPAA compliance certifications or undergo third-party audits to verify their adherence to HIPAA regulations.
- Evaluate Data Handling Practices: Assess how the provider handles data backups, disaster recovery plans, and retention policies to ensure data integrity and availability.
- Read Their Privacy Policy: A transparent privacy policy should outline how patient data is collected, stored, and used, aligning with HIPAA standards.
By examining these factors, you can select a form provider that meets the strict requirements of HIPAA compliance with confidence. There are a multitude of form builders available in the market. MakeForms is one such HIPAA-compliant form builder that you can use!
MakeForms – An Intuitive & HIPAA-Compliant Form Builder
MakeForms is a digital form building solution, designed to streamline, modernize, and simplify your medical data collection process. Most importantly, it does all that while ensuring HIPAA compliance. With a robust array of features tailored for healthcare professionals, MakeForms untangles form creation with its intelligent Form Builder.
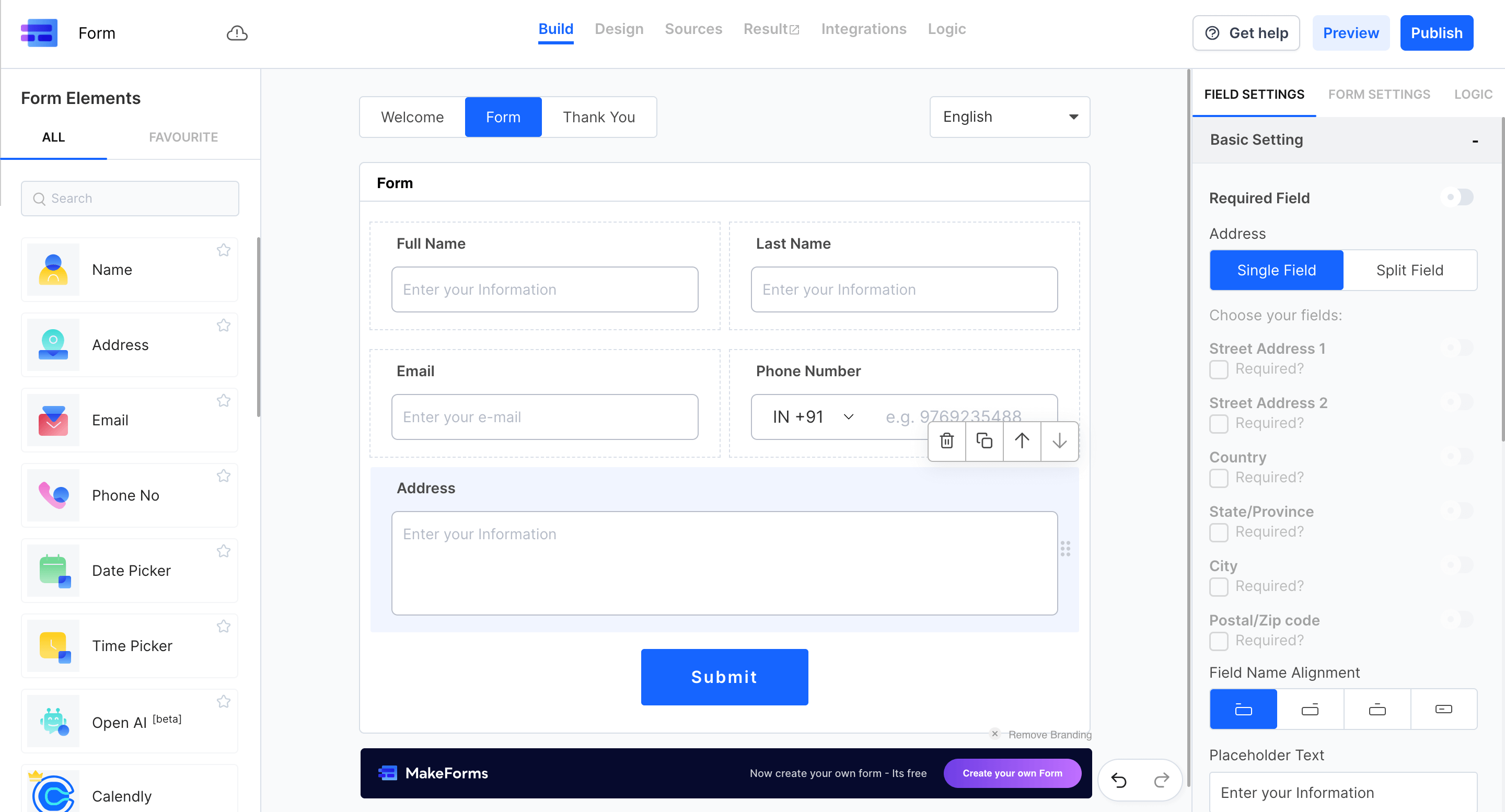
Craft custom forms effortlessly with a diverse range of Form Fields and unleash advanced features, like:
- Conditional Logic and Workflows to tailor form experiences based on user responses
- Custom Branding and Domain Mapping to maintain your professional image seamlessly
- Collaboration features for effortless team coordination
- Sharing or Embedding forms and Verified Submissions for added security
With many other features, MakeForm empowers you to collect, manage, and do so much more with medical data.
Book a demo to experience the convenience of MakeForm and elevate your medical form processes today.
FAQs
HIPAA stands for Health Insurance Portability and Accountability Act, a law enacted in 1996 to protect sensitive patient health information.
HIPAA-compliant forms ensure the privacy and security of patient information, mitigating risks of data breaches and legal penalties.
Healthcare providers, health plans, clearinghouses, business associates, medical labs, and pharmacies handling protected health information (PHI) are required to use HIPAA-compliant forms.
Failing to use HIPAA-compliant forms can result in financial penalties, corrective action plans, civil lawsuits, criminal charges, and reputational damage for healthcare organizations.